You can revolutionize surgical instrument development by leveraging 3D printing technologies like SLA, SLS, and DMLS to create patient-specific prototypes in days rather than months. You’ll need biocompatible materials meeting ISO 10993 standards, including medical-grade polymers and metals like titanium. Focus on self-supporting geometries, adequate wall thickness, and modularity while ensuring proper sterilization processes. Consider regulatory compliance, intellectual property protection, and cost savings that can reduce development expenses considerably. This all-encompassing approach will transform your entire prototyping workflow.
Advantages of 3D Printing for Surgical Instrument Development
While traditional surgical instrument manufacturing can take months or even years to bring a new design to market, 3D printing revolutionizes this process by enabling rapid prototyping that reduces development time from months to mere days.
You’ll find that this technology creates patient-specific instruments tailored to individual surgical needs, enhancing surgical precision considerably.
The design flexibility offered allows you to produce complex geometries impossible with conventional methods, fostering innovation in surgical practices.
Additionally, you’ll benefit from dramatically reduced production costs by eliminating expensive tooling and setup requirements.
3D printing eliminates costly tooling and setup expenses, delivering significant production savings for surgical instrument manufacturing.
Modern biocompatible materials guarantee your printed instruments meet stringent safety standards while maintaining durability.
This combination of speed, customization, and cost-effectiveness transforms how you approach surgical instrument development.
Essential 3D Printing Technologies for Medical Prototyping
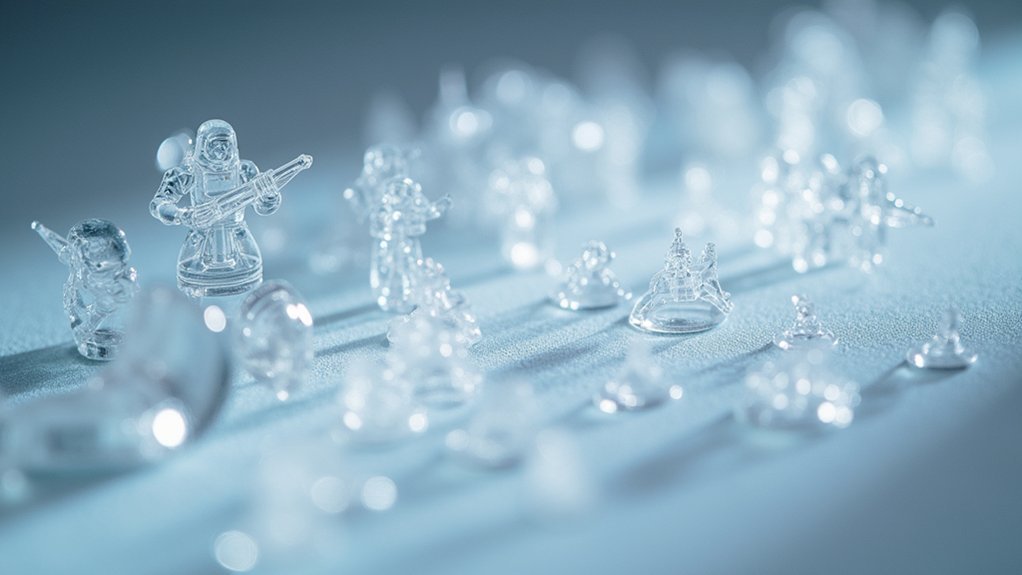
Understanding these advantages leads directly to selecting the right 3D printing technology for your medical prototyping needs.
When developing surgical instruments, you’ll find SLA technology excels at producing high-resolution prototypes with smooth surfaces and intricate details.
For testing mechanical properties, SLS uses laser fusion to create durable, functional prototypes from powdered materials.
FDM offers cost-effective rapid prototyping with excellent material versatility for full-scale instruments.
DLP delivers faster print times than SLA while maintaining exceptional resolution for detailed medical applications.
When you need robust, biocompatible surgical instruments that meet stringent mechanical requirements, DMLS and other metal 3D printing technologies become essential.
Each technology serves specific prototyping requirements in surgical instrument development.
Material Selection and Biocompatibility Requirements

Once your prototyping technology is selected, material selection becomes the cornerstone of successful surgical instrument development.
Material selection forms the foundation upon which all successful surgical instrument prototypes are built.
You’ll need to prioritize biocompatibility following ISO 10993 standards to guarantee patient safety and prevent adverse tissue reactions. Medical-grade polymers like Nylon and PEEK offer excellent options, while metals such as titanium and stainless steel provide superior strength and durability for demanding applications.
You must evaluate mechanical properties including Young’s modulus and tensile strength to guarantee your surgical instruments perform comparably to traditional tools.
Don’t overlook post-processing requirements—sterilization methods like gamma radiation are essential for clinical safety.
Finally, you’ll need thorough documentation for regulatory compliance, whether pursuing FDA 510(k) clearance or CE marking approval.
Design Considerations for Functional Surgical Prototypes
Since structural integrity directly impacts surgical performance, you’ll need to design prototypes with self-supporting geometries that eliminate or minimize support structures during printing. This approach reduces post-processing time while maintaining the strength vital for surgical applications.
You must guarantee adequate wall thickness in your functional prototypes to prevent deformation during use. Design considerations should include modularity, allowing easy assembly and disassembly of components for maintenance and adaptability in surgical environments.
Integrate measurement features and test points into your designs to streamline validation processes. When selecting biocompatible materials, prioritize advanced resin options that meet regulatory standards.
These design considerations guarantee your prototypes deliver reliable performance while maintaining the safety requirements essential for surgical instrument development.
Workflow for Creating Surgical Instrument Prototypes
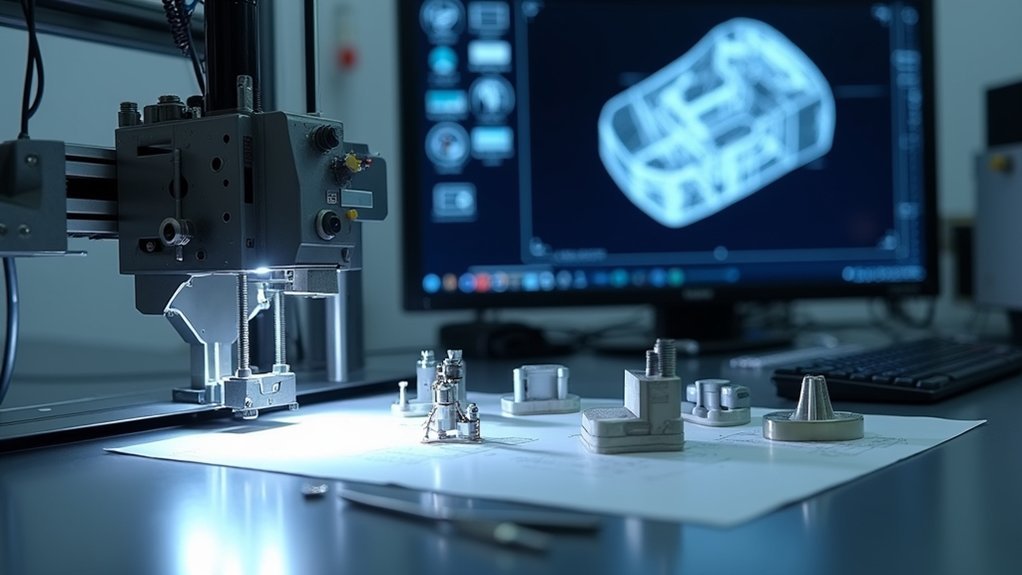
With your design principles established, implementing an effective workflow becomes the foundation for successful surgical instrument prototyping.
You’ll start by acquiring patient data through 3D medical imaging to capture precise anatomical information. This data drives your design generation, whether you’re creating prototypes manually or using automated processes tailored to specific surgical requirements.
Your manufacturing phase offers flexibility through direct printing or indirect methods like custom tooling.
Manufacturing flexibility empowers surgical teams through direct 3D printing capabilities or traditional indirect methods using specialized custom tooling systems.
You’ll gather feedback from surgeons throughout development to refine your surgical instruments. Critical post-processing steps, including sterilization, guarantee your prototypes meet safety standards for surgical applications.
This streamlined workflow minimizes in-surgery adjustments, delivering functional medical prototypes that enhance surgical efficiency and effectiveness while maintaining the highest quality standards.
Rapid Iteration and Testing Methodologies
As you shift from prototype development to refinement, rapid iteration becomes your most powerful tool for perfecting surgical instrument designs. Through 3D printing, you’ll produce functional prototypes within hours, enabling immediate testing methodologies and design feedback from surgeons. This prototyping process dramatically reduces your time to market while minimizing traditional manufacturing costs.
| Testing Phase | Timeline | Output |
|---|---|---|
| Initial Prototype | 2-4 hours | Basic functionality test |
| Design Refinement | 1-2 hours | Surgeon feedback integration |
| Final Validation | 3-5 hours | Performance verification |
Advanced printing technologies like SLA and SLS let you create complex geometries with precise details essential for surgical instruments. You’ll identify design flaws early, make quick adjustments, and produce full-scale prototypes that mimic final product performance—all without expensive tooling or lengthy manufacturing delays.
Quality Control and Validation Processes
When your 3D printed surgical instrument prototypes demonstrate promising functionality, you must implement rigorous quality control and validation processes to confirm they meet stringent medical standards.
You’ll need to establish a robust quality management system following regulatory guidelines like FDA requirements and ISO 13485:2016 certification.
Your validation processes should include thorough biocompatibility testing according to ISO standards, confirming materials are safe for medical applications.
Through iterative testing, you’ll identify and address design flaws while documenting all results for compliance tracking.
Integrating feedback from surgeons during validation enhances instrument reliability and functionality.
You should employ advanced quality control methods, including real-time monitoring and data-driven analysis, to support continuous improvement and confirm your final products meet exceptional performance and safety standards.
Regulatory Compliance for Medical Device Prototypes
Before you can advance your 3D printed surgical instrument prototypes toward clinical use, you must navigate complex regulatory frameworks that govern medical device development.
You’ll need to establish robust quality management systems that comply with FDA regulations under 21 CFR Part 820 and ISO 13485:2016 for European markets.
Your regulatory compliance strategy requires implementing traceable design processes that document every development phase.
You must conduct thorough biocompatibility testing to demonstrate material safety based on your device’s intended contact type.
Testing and validation procedures are essential to verify your prototypes meet established performance metrics.
These rigorous design processes enhance your credibility with regulators and enable effective risk management throughout development.
Proper documentation of your medical device prototypes ensures smoother pathways to market approval.
Cost Analysis and Production Scalability
While regulatory compliance establishes the foundation for bringing 3D printed surgical instruments to market, understanding the economic implications and production scalability becomes critical for sustainable implementation.
You’ll find cost compared to traditional surgical instruments greatly favors 3D printing, with instrument trays exceeding $50,000 versus in-house production alternatives. Custom surgical instrument prototypes requiring hours instead of weeks considerably compress your development timeline while enabling rapid design iterations based on surgeon feedback.
Production scalability improves through accessible equipment like Formlabs printers, offering lower initial investments for medical device manufacturers.
You’ll reduce supply chain dependency and sterilization costs through localized production capabilities. This economic advantage allows small to mid-sized manufacturers to compete effectively while maintaining quality standards and meeting specific surgical requirements.
Intellectual Property Protection and Legal Considerations
When you’re developing 3D printed surgical instruments, you’ll need to establish clear patent filing strategies that protect your innovations while considering the rapid pace of technological advancement in this field.
You must also implement robust trade secret management protocols to safeguard proprietary manufacturing processes, material formulations, and design specifications that give you competitive advantages.
Additionally, you’ll want to carefully structure licensing agreements that balance revenue opportunities with maintaining control over how your intellectual property is used by partners or competitors.
Patent Filing Strategies
As you develop innovative 3D printed surgical instruments, protecting your intellectual property becomes paramount to securing competitive advantages and preventing unauthorized replication of your designs.
Your patent filing strategy must demonstrate novelty, non-obviousness, and utility to achieve effective legal protection.
Here’s your strategic approach:
- Conduct thorough prior art search – Identify existing patents to determine your design’s uniqueness and reduce infringement risks before filing applications.
- File provisional patent applications – Secure early filing dates while allowing 12 months for prototype refinement and medical device technology development before submitting full applications.
- Document design process meticulously – Record iterations, testing results, and development timeline to establish credibility and demonstrate your invention’s effectiveness.
Engaging a patent attorney experienced in medical device technology guarantees compliance with regulatory requirements and maximizes your patent approval chances.
Trade Secret Management
A fortress of confidential information surrounds your 3D printed surgical instrument innovations, and you’ll need robust trade secret management to keep competitors from accessing your proprietary designs, manufacturing processes, and specialized materials.
You’ll protect these proprietary processes through non-disclosure agreements with employees and partners handling sensitive information. Implement intellectual property policies alongside regular employee training to guarantee your team understands their role in safeguarding confidential data.
Establish monitoring and auditing systems to track information access and identify potential leaks before they compromise your innovations. Developing an all-encompassing trade secret strategy that combines documentation, legal safeguards, and training protocols will strengthen your competitive advantage in 3D printing for surgical instruments while securing your most valuable technological assets.
Licensing Agreement Considerations
Beyond securing your proprietary information through trade secrets, you’ll face complex decisions when entering licensing agreements for your 3D printed surgical instrument innovations.
These contracts determine how your intellectual property gets used while protecting your competitive advantages.
Your licensing agreements must address three critical areas:
- IP ownership and confidentiality clauses – Define who owns what innovations and establish strict confidentiality clauses protecting proprietary information throughout the partnership.
- Regulatory compliance verification – Guarantee your licensing partner meets quality management standards and safety and efficacy requirements for surgical instruments before production begins.
- Financial terms structure – Establish clear royalties and profit-sharing arrangements that reflect your technology’s value while incentivizing proper development of your innovations.
Thorough due diligence protects both your intellectual property and patients who’ll ultimately use these surgical instruments.
Frequently Asked Questions
Can 3D Printed Surgical Instruments Be Sterilized Using Standard Hospital Methods?
You can’t sterilize most 3D printed surgical instruments using standard hospital methods. The plastic materials typically degrade under autoclave temperatures, and porous surfaces from printing can harbor bacteria even after sterilization attempts.
How Long Do 3D Printed Surgical Instrument Prototypes Typically Last?
You’ll find prototype lifespans vary dramatically based on materials and usage. PLA prototypes last days to weeks, while PEEK can endure months. Your prototype’s durability depends on stress testing, sterilization cycles, and intended application requirements.
What Training Do Surgeons Need to Use 3D Printed Instruments?
You’ll need specialized training on the instrument’s unique properties, handling characteristics, and safety protocols. Most hospitals require certification courses covering 3D-printed material behavior, sterilization procedures, and emergency protocols before you can use them.
Are There Insurance Coverage Considerations for 3D Printed Surgical Tools?
You’ll face significant insurance challenges with 3D printed surgical tools. Most insurers don’t cover experimental devices, requiring extensive FDA approval documentation and clinical evidence to demonstrate safety and efficacy for potential reimbursement.
Can Patients Request Custom 3D Printed Instruments for Their Surgery?
You can’t directly request custom 3D printed instruments for your surgery. Your surgeon decides which tools are appropriate based on medical necessity, regulatory approval, and their professional judgment regarding safety.



Leave a Reply